
What is ME?
Myalgic Encephalomyelitis (ME) is a long-term, fluctuating disease that causes symptoms affecting many body systems.
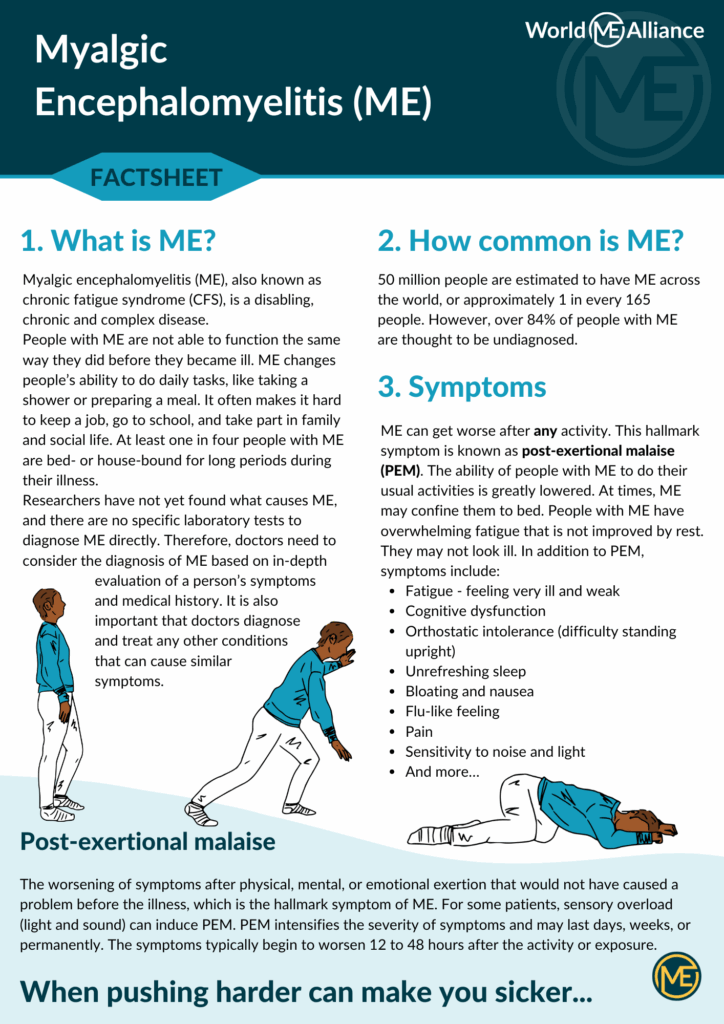
The hallmark symptom of ME is post-exertional malaise. This is a worsening of symptoms after physical, mental, or emotional exertion that would not have caused a problem before the illness. For some patients, sensory overload (light and sound) can induce PEM. PEM intensifies the severity of symptoms and may last days, weeks, or permanently. The symptoms typically begin to worsen 12 to 48 hours after the activity or exposure.
Quick ME facts
The ME Factsheet
What are the symptoms?
Symptoms vary from person to person, and there are many different definitions of ME used across the world.
All recent diagnostic criteria include post-exertional malaise as a defining feature of ME. This is a global increase in symptoms following any type of exertion, including physical exercise, cognitive exertion (concentration), and emotional exertion such as stress. This reaction to exertion is often delayed by 24-48 hours, and can sometimes lead to a permanent worsening of the person’s condition – known as a relapse.
Other symptoms include:
- Cognitive dysfunction (commonly known as brain fog in English)
- Pain, including muscle and joint pain, and headaches
- Unrefreshing sleep
- Orthostatic Intolerance (difficulty being upright)
- Fatigue and muscle fatiguability
- Gastrointestinal symptoms such as bloating and nausea
- Sensitivity to noise, light and smell
- Flu-like symptoms such as a sore throat
There are many more possible symptoms that ME can cause. Each person with ME will have different symptoms or severity of symptoms.
Who Gets ME/CFS?
Everyone is at risk. Although research has shown that ME/CFS is about two to four times more likely to occur in women than men, ME strikes people from every age, racial, ethnic, and socioeconomic group. Some studies show that ME/CFS may be more common in minority groups.
How is ME treated?
There is currently no universally effective treatment for ME. As neither a cause nor cure for ME has been identified, treatment is directed at relieving symptoms. Although there’s no single effective treatment that addresses the disease at its core, there are treatments that can improve symptoms and increase functioning in some. Different countries have different approaches to treating ME, so take a look at our members page to see if an organisation in your country can provide more information.
How severe is ME?
Research shows that people with ME have lower health-related quality of life scores than most other chronic conditions, including multiple sclerosis, systemic lupus erythematosus, rheumatoid arthritis, congestive heart failure and various cancers.
25% of people with ME are housebound or bedbound.
There are a few different severity scales used to categorise how severe ME is. Most use either a 3 point or 4 point scale. Here is one way of looking at severity:
Mild
Mobile and self-caring; may continue working but will have reduced other activities
Moderate
Reduced mobility, restricted in instrumental activities of daily living, needs frequent periods of rest; usually not working
Severe
Mostly housebound; limited to minimal activities of daily living (eg, face washing, showering); severe cognitive difficulties; may be wheelchair dependent
Very Severe
Mostly bedridden; unable to independently carry out most activities of daily living; often experience extreme sensitivity to light, sound, and other sensory input
This scale is taken from Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Essentials of Diagnosis and Management, developed by the ME/CFS Clinicians Coalition. Other severity scales include the Bell Disability Scale, and the ME Disability Scale by Dr Charles Shepherd.
Different names
ME (myalgic encephalomyelitis) has been given various different names over the years. These include chronic fatigue syndrome (CFS), ME/CFS, myalgic encephalopathy and systemic exertion intolerance disease (SEID).
Each of these different names also relates to a different diagnostic criteria. We use ME because this is what most English speaking people with ME use, however we recognise that CFS is still commonly used in countries across the world.
Many people believe that the name chronic fatigue syndrome underplays the seriousness of this disease.
Another diagnosis given to many is post-viral fatigue syndrome (PVFS), however this is usually considered a self limiting illness, and if people don’t recover they are often then given an ME or CFS diagnosis.
More research needs to be done to understand the different subgroups of people who receive an ME, CFS, ME/CFS, PVFS or SEID diagnosis. We will always advocate for all of these people, and consider it important to leave no-one behind, even as research advances.
